Category: Uncategorized
Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study
British Journal of Sports Medicine
Executive Summary
Adults who engaged in the recommended levels of physical activity (including a combination of aerobic and resistance training) of at least 150 mins per week (or more precisely – metabolic equivalent task (MET; 500–1000 MET min/ week) were associated with a decreased likelihood of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related death. Our findings suggest that engaging in physical activity has substantial public health value and demonstrates potential benefits to combat COVID-19.
Continue reading...
My experience of changing from long-term drug treatment of rheumatoid arthritis to following a more natural approach (2012 – 2021) – by Rosemary Wellman
In 2012, I was unexpectantly diagnosed with rheumatoid arthritis, an auto-immune disease, at Charing Cross Hospital, which, fortunately for me had an excellent Rheumatology department. I was immediately prescribed the steroid Prednisolone for a couple of months, which really helped control the inflammation and pain effectively. I was also monitored regularly with blood tests. I was able to carry on working and traveling at that stage.
In 2013, the next stage involved being prescribed DMards (disease-modifying anti-immune drugs) i.e Sulfasalazine and Hydroxychloroquine, the latter having become notorious during ex-President Trump’s time. These enabled me to carry on working and traveling for some time.
Diet and fitness with rheumatoid arthritis
I had always had a healthy diet, my weight had been a constant 52 kg, (height 5’7). I’d also been playing badminton and going to Pilates classes every week when I had my diagnosis. With this in mind, in 2012, I had asked the Rheumatologist for her advice on self-help to ease the worst effects of RA. Her immediate response was that I should follow the Mediterranean diet as much as possible, as it’s generally anti-inflammatory.
What is generally referred to as a Mediterranean diet is based mainly around vegetables, fruits, whole grains, nuts and seeds, healthy fats, eggs, poultry, red meat, fish rich in omega-3, and as much extra virgin olive oil as possible!
After doing some research and from personal experience, I found some foods I should be avoided which can make the inflammation and other symptoms of RA worse, these are white bread, white rice, margarine, cereals, potatoes, polyunsaturated cooking oil, processed and sugary foods.
Rheumatoid Arthritis Remission
In 2016, I was told I was in remission, which was good news, although I was still taking theDMard drugs, which I thought were pretty toxic. I decided maybe it was time to think about winding them down and eventually managing without them. This was not encouraged by my rheumatologist, who carried on prescribing the same drugs more or less to the present day.
Also in 2016, I had a spell in Sussex County hospital after suffering a minor stroke and heart problems. Up until then, I’d kept my fitness and maintained the same weight ever since my diagnosis, I then began cardiac rehab exercises held in the hospital.
After being discharged, I moved on to phase IV cardiac rehab exercise classes (specific to cardiac recovery) run by the qualified trainer and exercise physiologist, Richard Stantiford. I am still following these regular cardiac rehab exercise classes which also help reduce the pain and inflammation from the RA. (see link below), as well as improving my balance and stability following the stroke.
htps://thelifestylephysiologist.com/exercise-benefits-in-cardiovascular-disease-new-findings/
With my aim of coming off the drugs and supporting the ‘food as medicine’ healthy lifestyle, I was pleased when Richard invited me to become a co-founder of the website he founded in 2019 the Lifestyle Physiologist. I have learned a lot from him and have much faith in his methods. It is thanks to Richard’s exercise regime, that I have managed to keep the RA in remission, as shown on my recent blood tests.
By chance, recently, when trying to refill my prescription for Sulfasalazine, I was told none was available and even Pfizer, the manufacturer, had run out. For some time before this, I had been taking Turmeric as a supplement, along with Vitamin D, and on checking with my consultant, have been given the ok to stop taking Sulfasalazine, with the possibility, if I remain well and in remission, that the hydroxychloroquine can go too.
To Sum up briefly, With my ultimate goal of reducing the drugs I’ve been taking for rheumatoid arthritis for so long, although It’s been a long haul, I now feel much better knowing that I am in control of my body and health, rather than any drugs.
footnote: I have worked out, in the ten years I’ve been taking the RA drugs, I’ve taken over 16,000 pills!
Author: Rosemary Wellman – Co-founder The Lifestyle Physiologist
Continue reading...
TLP Cardiac Exercise via Zoom – One Year Anniversary
8th April 2021
This morning whilst beginning another cardiac exercise session via Zoom I was reminded by one of my loyal members (Jen) that we had been going for just over a year since the first Lockdown. I never would have imagined that firstly I would be running online cardiac rehab exercise at all, and second that it would have proved to be so successful as well as being adhered to by virtually everyone a year down the line (long term exercise adherence is generally very poor).
The feedback and enthusiasm I have received from my regular participants throughout has been tremendous and has undoubtedly helped to keep me feeling more positive during this difficult period, although I’m not ashamed of admitting I’ve had some real low points as well as a lingering fear about whether or not I could earn enough to cover the mortgage, bills and provide for my children – especially little Olivia who is only 17 months old now.
Here is just one example of some of the feedback that has given me a real boost…
“What a lifesaver Richard’s Zoom Cardiac exercise classes have been during this Covid period. Not only ensuring a well needed routine of brilliantly run 4 x morning sessions per week, which has improved my personal fitness greatly to the point, I am far much more healthier now than when I started! How many people locked down for so long can say that? The enormous professionalism and style of Richard’s classes, ensuring each exercise can be done by all levels of fitness and mobility, by his great demonstrations for each level of our attendees ability is so magic. No-one is left out from the unfit learner to the fit experts. I do so look forward daily now to each session, catching up live with the other class members who have become great friends. We so enjoy our chats and banter prior to Richard starting the warm-up session and also at the end of the lessons. What really sets Richard’s lessons apart from other instructors is his massive qualifications and cardiac rehabilitation knowledge we all benefit greatly from whether it be about our medication or symptoms advice and also arranges Cardiologist Webinars for us. All this and much more like any equipment we might like, eg small weights, can be purchased at bargain prices from him and his prices are the most competitive on the market. A life-saving bargain. It does not get any better than that!” Phil Careless, Hove
Following the first lockdown my job as ‘Lead Cardiac Rehab Exercise Physiologist’ for the charity (Take Heart Group) that I have dedicated the last 16 years to, suddenly ceased to exist. Now without any regular income and an awareness that many of my patients that I was used to seeing face to face would be anxious to know what they would do now to keep themselves fit and healthy we piloted a small online exercise class.
We started off with about 10 people and this has grown to around 35 regulars, whom frequently tell me it has given them structure and a daily routine, social connection, safety from Covid-19, much improved fitness and wellbeing, and an interactive platform to ask health related questions or share concerns about the pandemic. Perhaps most importantly we have a bit of a laugh and a joke and mostly try to avoid heated medical or political debates, as this pandemic has undoubtedly created some polar opposite viewpoints.
We could have helped many more recovering cardiac patients throughout lockdown but sadly our efforts were not supported or promoted locally. In fact one new patient told me that all he was offered was a phone call and a sheet of exercises to follow – which he said was incredibly uninspiring and he didn’t continue with. I’m not sure how this approach is somehow safer or more effective than an interactive zoom class with an instructor with 17 years cardiac rehab experience?
Anyway with the help of my web designer (Gavin Reynoldson) and some input from my very dear friend, and client Rosemary Wellman we launched the Lifestyle Physiologist website – which has already received 8 FIVE STAR GOOGLE REVIEWS despite only being in existence for a few months.
To kick off January 2021 – we also delivered a hugely successful Webinar with award-winning Cardiologist – Dr Aseem Malhotra on “ How to optimise your Cardiovascular and Metabolic Health” with over 200 attendees.
This event included a fascinating presentation from the Doc and was followed by a 90-minute Q&A. We received an enormous amount of positive feedback following this event, which made it all worthwhile organising.
Now with the vaccine roll out – virtually all of the clinically vulnerable and those over 60 years have some hope that we are heading out of this disaster. Herd immunity is apparently reached on Monday 12th of April which is encouraging. Although there is talk of reopening group exercise classes in May – how practical or safe that will be for people with chronic diseases like heart disease, diabetes or obesity remains to be seen.
For now, my participants inform me that they wish to carry on with the online circuits indefinitely, although I haven’t ruled out the possibility of running indoor group cardiac exercise later this year.
All the best,
Richard
Continue reading...
Hi, folks so I wanted to share with you this particular review written by Dr Zoe Harcombe who is a friend of mine but more importantly is a researcher, author, and public speaker in the field of diet and health, with a PhD in public health nutrition. She has quite rightly pointed out the importance of Vitamin D status and Covid-19 risks and yet NICE and the NHS seem to be completely ignoring the evidence saying that it’s of “low quality”.
Well, Zoe is someone that I respect and trust to go through the evidence with a fine-tooth comb (with no bias or conflicts of interest) so you have to ask the question: If there are no downsides to supplementing with Vitamin D (especially in winter) only positive health outcomes that could potentially save your life if you got Covid – Why on earth would you not be recommending this cheap and easy fix to the general public?
NICE, Vitamin D & Covid-19
Executive Summary
* The UK National Institute for Care & Health Excellence (NICE) undertook a rapid review of vitamin D for the treatment and prevention of Covid-19. The review was published in December 2020.
* Three research questions were asked about 1) vitamin D as a treatment for Covid-19, 2) vitamin D for prevention of Covid-19 and 3) any associations observed between vitamin D and Covid-19 outcomes.
* NICE found one randomised controlled trial (RCT) to consider for question 1, no RCTs for question 2 and 12 population/case control type studies for question 3.
* The one RCT examining vitamin D for treatment of Covid-19 found that administration of vitamin D at hospital admission significantly reduced the likelihood of being admitted to ICU and no one treated with vitamin D died. The odds ratios were striking.
* The 12 studies examining the association between vitamin D levels and incidence of Covid-19 and/or severity of Covid-19 (including survival from) were conducted in many different countries by many different research teams. Vitamin D levels were reviewed as absolute levels and as deficient or sufficient levels.
* Two UK studies (using Biobank data) found nothing statistically significant. The other 10 studies all concluded that higher/sufficient vitamin D levels were associated with significantly better outcomes from Covid-19. The risk ratios for lower/insufficient vitamin D levels were striking in many cases – up to 15-fold difference in one study and often beyond the 2-fold difference used as a starting point for causality with the Bradford Hill criteria.
* Every single study, every single piece of evidence, was dismissed in the NICE document as “very low” in quality and at “serious risk of bias” or “very serious risk of bias.”
* I saw a lot of evidence to support vitamin D being a valuable intervention to lessen the likelihood of bad outcomes (including death) from Covid-19. NICE essentially concluded “move along – there’s nothing to see here.”
Introduction
The UK National Institute for Care & Health Excellence (NICE) undertook a rapid review of vitamin D for the treatment and prevention of Covid-19. The review was published in December 2020 (Ref 1). The committee undertaking the work asked three research questions:
Research questions
1) What is the clinical effectiveness and safety of vitamin D supplementation for the treatment of Covid-19 in adults, young people, and children?
2) What is the clinical effectiveness and safety of vitamin D supplementation for the prevention of SARS CoV2 infection (and subsequent Covid-19) in adults, young people, and children?
3) Is vitamin D status independently associated with susceptibility to developing Covid-19, severity of Covid-19, and poorer outcomes from Covid-19 in adults, young people, and children?
The three key words in these research questions are 1) treatment 2) prevention and 3) association. The search for evidence was conducted on the period 2002 to October 27th, 2020. This allowed for other coronaviruses, such as SARS CoV1 (symptomatic) and MERS, to be included as indirect evidence. It transpired that only Covid-19 studies were included.
Outcomes of interest
The main outcomes of interest for research questions 1 and 2 were mortality (all-cause and Covid-19 related) and Intensive Care Unit (ICU) admissions. There were a number of secondary outcomes of interest including hospitalization, ventilation, time to clinical cure, complications, and others. I haven’t listed all the secondary outcomes of interest because, as you will see, only one study ended up being considered as evidence for Question 1 and no studies ended up being considered as evidence for question 2.
The outcomes of interest for research question 3 were:
– Incidence of Covid-19 (laboratory/virologically confirmed)
– Covid-19 rate (laboratory/virologically confirmed)
– Severity of confirmed Covid-19 (for example, but not limited to, Centers for Disease Control and Prevention definition, World Health Organization definition, proxy such as hospitalisation, ventilation, ICU admission, and others)
– Poor outcomes (for example, mortality, complications, morbidities post infection, long Covid).
Inclusion & exclusion criteria
The inclusion criteria for research questions 1 and 2 were: systematic review of randomised controlled trials (RCTs); RCTs; and controlled clinical trials. The exclusion criteria for research questions 1 and 2 were: case-control studies; cross section studies; case series and case reports; and qualitative studies (Ref 2).
The inclusion criteria for research question 3 were: systematic review of non-randomised studies; prospective and retrospective cohort studies; case-control studies; cross-sectional studies; and case series. The exclusion criteria for research question 3 were case reports.
Studies found meeting criteria
For research question 1, one study was included (Entrenas Castillio et al 2020 RCT Spain) (Ref 3).
For research question 2, no studies were included.
For research question 3, 12 studies were included (see below).
I checked the studies found with a vitamin D expert, who knows the literature far better than I do, and he thought that the committee had found the studies that met their criteria. I am proceeding on the basis that the studies available for each of these research questions are as presented in the report.
The results
Research question 1
The one study included to answer this research question was conducted in a hospital in Spain. This study involved 76 patients who were hospitalised with lab-confirmed Covid-19. They were randomised in a 2:1 ratio to the treatment arm or the control arm; so 50 people ended up in the treatment arm and 26 in the control arm. The treatment was administration of oral calcifediol (vitamin D3) (0.532 mg) on the day of admission. Patients in the calcifediol treatment group continued with oral calcifediol (0.266 mg) on days 3 and 7, and then weekly until discharge or ICU admission. People in the control arm were not given any vitamin D. Other treatment between the patients remained the same.
Of the 50 patients treated with calcifediol, 1 required admission to ICU (2%) while, of 26 untreated patients, 13 required admission (50%). That was a statistically significant and clinically significant difference. Of the patients treated with calcifediol, none died, and all were discharged without complications. The 13 patients not treated with calcifediol, who were not admitted to the ICU, were discharged. Of the 13 patients admitted to the ICU, 2 died and the remaining 11 were discharged.
The odds ratio (OR) for ending up in ICU was 0.02 (95 %CI 0.002−0.17) for the treatment group vs the no-treatment group. That was almost a 0% chance of the vitamin D group ending up in ICU. When the results were adjusted for differences between the two groups for hypertension and type 2 diabetes, the odds ratio was still 0.03 (95 %CI: 0.003-0.25).
The NICE document dismissed this evidence as “very low” in quality and at “very serious risk of bias” for ICU admission and as “very low” in quality and at “very serious risk of bias” for mortality.
Research question 2
NICE found nothing to examine for the research question about prevention.
Research question 3
NICE found 12 studies to help with the research question – is there any evidence for vitamin D being associated with developing Covid-19 or the severity of Covid-19 if diagnosed? The 12 studies were all from 2020. Two studies each came from France, the UK, the US, and from Spain and one each came from China, Germany, Israel, and Turkey. The studies were mainly of population studies and case-control studies.
We’ll whizz through them – extracting the salient point from the original papers. (I’m going to keep numbers and confidence intervals to a minimum for ease of reading. All of these can be found in the paper abstracts, which the references can point you to. Many of the findings are so significant in the normal sense of the word, that confirmation of the statistical significance will just clutter the narrative).
1) Annweiler et al. Retrospective quasi-experimental study France (Ref 4).
The first Annweiler et al study involved 66 frail elderly residents in a French nursing home with an average age of 88. The intervention group was defined as all residents diagnosed with Covid-19 who received an oral dose of 80,000 IU vitamin D3 either in the week following the suspicion or diagnosis of Covid-19, or during the previous month. This definition placed 57 people in the intervention group and 9 in the control. 82.5% of participants in the Intervention group survived Covid-19, compared to 44.4% in the Comparator group.
The researchers concluded that vitamin D supplementation was independently associated with less severe Covid-19 and better survival rate.
The NICE document dismissed this evidence as “very low” in quality and at “very serious risk of bias.”
2) Annweiler et al. Retrospective cohort study France (Ref 5).
The second Annweiler et al study involved 77 patients hospitalised for Covid-19 in a geriatric unit with an average age of 88. Group 1 (29 people) regularly supplemented with vitamin D over the previous year. Group 2 (16 people) were supplemented with vitamin D after Covid-19 diagnosis and the comparator group (Group 3 – 32 people) received no vitamin D supplementation. In Group 1, 93% of Covid-19 participants survived at day 14, compared to 81% survivors in Group 2 and 69% survivors in Group 3.
The researchers concluded that vitamin D supplementation was independently associated with less severe Covid-19 and better survival rate.
The NICE document dismissed this evidence as “very low” in quality and at “very serious risk of bias.”
3) Hastie et al. Retrospective cohort study UK (Ref 6).
The Hastie et al study examined the UK Biobank data between 16th March and 14th April 2020 for lab confirmed Covid-19 and patient vitamin D levels. Complete data were available for 348,598 participants. Of these, 449 had confirmed Covid-19. After adjustments, vitamin D was not associated with infection rates. The most interesting finding is surely how low the incidence of Covid-19 was given that the peak of the UK Covid-19 curve was 8th April, 2020.
The researchers’ findings did not support a potential link between vitamin D concentrations and risk of Covid-19 infection.
The NICE document dismissed this evidence as “very low” in quality and at “very serious risk of bias.”
4) Hernández et al. Case-control study Spain (Ref 7).
The Hernández et al study examined 216 Covid-19 patients and 197 population-based controls (average age 60-61) to see if vitamin D levels were associated with the incidence of Covid-19. Vitamin D deficiency was found in 82% of Covid-19 cases and 47% of population-based controls (Ref 8).
The researchers concluded that vitamin D levels were lower in hospitalised Covid-19 patients than in population-based controls and that these patients had a higher prevalence of deficiency.
The NICE document dismissed this evidence as “very low” in quality and at “serious risk of bias.”
5) Karahan and Katkat. Case-control study Turkey (Ref 9).
The Karahan and Katkat study examined 149 patients (average age 64) hospitalised with Covid-19 for severity and/or mortality. 47 patients had moderate Covid-19; 102 patients were severe-critical. Average blood vitamin D levels were significantly lower in patients with severe-critical Covid-19, compared with moderate Covid-19 (Ref 10). Vitamin D insufficiency was present in 93% of the patients with severe-critical Covid-19.
The researchers concluded that vitamin D was independently associated with mortality in Covid-19 patients.
The NICE document dismissed this evidence as “very low” in quality and at “serious risk of bias.”
6) Kaufman et al. Retrospective cohort study US (Ref 11).
The Kaufman et al study examined over 190,000 patients (average age 54) from the 50 US states and matched them with vitamin D level results (25(OH)D) from the preceding 12 months. The SARS-CoV-2 positivity rate was higher (at 12.5%) in the 39,190 patients with “deficient” vitamin D (<20 ng/mL) than in the 27,870 patients with “adequate” vitamin D (30–34 ng/mL) (8.1%) and the 12,321 patients with values ≥55 ng/mL (5.9%). The association between 25(OH)D levels and SARS-CoV-2 positivity produced an R2 value of 0.96, which indicated strong correlation in the total population (strong is an understatement with an R2 of 0.96).
The researchers concluded that SARS-CoV-2 positivity was strongly and inversely associated with circulating vitamin D levels, a relationship that persisted across latitudes, races/ethnicities, both sexes, and age ranges.
The NICE document dismissed this evidence as “very low” in quality and at “very serious risk of bias.”
7) Macaya et al. Case series Spain (Ref 12).
The Macaya et al study examined 80 patients with lab confirmed Covid-19 seen at the emergency department of a hospital where recent vitamin D (25(OH)D) levels were known. Vitamin D deficiency was associated with an increased risk of developing severe Covid-19 (after adjusting for all relevant factors.) The odds ratio was 3.2 – which is beyond a level at which causation can start to be assessed.
The researchers concluded that vitamin D deficiency did show an association with severe Covid-19 infection.
The NICE document dismissed this evidence as “very low” in quality and at “very serious risk of bias.”
8) Meltzer et al. Retrospective cohort study US (Ref 13).
The Meltzer et al study examined 489 patients (average age 49) at an urban medical centre for whom vitamin D levels had been measured within the previous year. Between March 3rd, and April 10th, 2020, 71 of these patients tested positive for Covid-19. Vitamin D deficiency was defined as 25(OH)D < 20 ng/mL. Testing positive for Covid-19 was associated with vitamin D deficiency (relative risk 1.77) when compared with vitamin D sufficiency. Predicted Covid-19 rates in the deficient group were 21.6% vs 12.2% in the sufficient group.
The researchers concluded that vitamin D deficiency was associated with increased Covid-19 risk.
The NICE document dismissed this evidence as “very low” in quality and at “serious risk of bias.”
9) Merzon et al. Case-control study Israel (Ref 14).
The Merzon et al Israeli study examined 14,000 members of a health service who were tested for Covid-19 between Feb 1st, and April 30th, 2020, who had at least one previous blood test for their 25(OH)D level. Suboptimal vitamin D levels in this study were defined as < 30 ng/mL. The 782 people who tested positive for Covid-19 had significantly lower average vitamin D levels. People with low vitamin D levels had an increased likelihood of Covid-19 infection (1.58 times) and increased likelihood of hospitalization (2.09 times).
The researchers concluded that “low plasma 25(OH)D levels appear to be an independent risk factor for COVID-19 infection and hospitalization.”
The NICE document dismissed this evidence as “very low” in quality and at “serious risk of bias.”
10) Radujkovic et al. Retrospective cohort study Germany (Ref 15).
The Radujkovic et al study examined 185 patients diagnosed with Covid-19 who presented at a German health centre. Vitamin D status was assessed at the time of admission. Vitamin D (25(OH)D) deficiency was set at a low bar of < 12 ng/mL. During an average period of 66 days, 93 patients required hospitalisation; 28 patients had a severe outcome (IMV/D – invasive mechanical ventilation and/or death). Among these 28 severe outcomes, there were 16 deaths. A total of 41 patients were vitamin D deficient. When adjusted for age, gender, and comorbidities, vitamin D deficiency was associated with higher risk of IMV/D and death. The risk ratios were 6.12 for IMV/D and 14.73 for death.
The researchers concluded that “our study demonstrates an association between vitamin D deficiency and severity/mortality of COVID-19.”
The NICE document dismissed this evidence as “very low” in quality and at “serious risk of bias.”
11) Raisi-Estabragh et al. Nested case-control study UK (Ref 16).
The Raisi-Estabragh et al studywas the second study to use the UK Biobank data. This study specifically examined men and Black, Asian, and Minority Ethnic (BAME) individuals, as these were patients identified as at higher risk of a poor outcome from Covid-19 than women and non-BAME individuals. This study asked a different research question and I’m not sure that it should have been included. It sought to see if any factors (of which vitamin D was just one) could explain why men and BAME individuals were having worse outcomes.
A total of 4,510 people were assessed. The study confirmed “there was over-representation of men and BAME ethnicities in the COVID-19 positive group.” However, the study couldn’t explain why. The conclusion was: “In this study, sex and ethnicity differential pattern of COVID-19 was not adequately explained by variations in cardiometabolic factors, 25(OH)-vitamin D levels or socio-economic factors.”
This mattered little anyway as the NICE document dismissed this evidence as “very low” in quality and at “very serious risk of bias.”
12) Ye et al. Case-control study China (Ref 17).
The Ye et al study compared the vitamin D (25(OH)D) levels and rates of vitamin D deficiency between 80 healthy controls and 62 patients diagnosed with Covid-18 and admitted to a hospital in China. Cases were categorized into asymptomatic, mild/moderate, and severe/critical disease. The vitamin D concentration in Covid-19 patients was much lower than that in healthy controls. Vitamin D levels were the lowest in severe/critical cases, compared with mild cases. Significantly higher rates of vitamin D deficiency were found in Covid-19 cases (42%) compared to healthy controls (11%). Vitamin D deficiency was the greatest in severe/critical cases (80%), compared with mild cases (36%).
The researchers concluded that vitamin D was associated with Covid-19 severity and added “a potential threshold of 25(OH)D (41.19nmol/L) to protect against COVID-19 was identified.”
The NICE document dismissed this evidence as “very low” in quality and at “very serious risk of bias.”
Summary
The one RCT examining vitamin D for treatment of Covid-19 found that administration of oral calcifediol (vitamin D) at hospital admission significantly reduced the likelihood of being admitted to ICU and no one treated with vitamin D died. The odds ratios were striking.
There were 12 studies (largely population and case control studies) examining the association between vitamin D levels and incidence of Covid-19 and/or severity of Covid-19 (including survival from). The studies were conducted in many different countries by many different research teams. Vitamin D levels were reviewed as absolute levels and as deficient or sufficient levels. The two UK studies using Biobank found nothing statistically significant. The other 10 studies all concluded that higher/sufficient vitamin D levels were associated with significantly better outcomes from Covid-19. The risk ratios for lower/insufficient vitamin D levels were striking in many cases – up to 15-fold difference in one study and often beyond the 2-fold difference used as a starting point for causality with the Bradford Hill criteria (Ref 18).
Every single study, every single piece of evidence, was dismissed in the NICE document as “very low” in quality and at “serious risk of bias” or “very serious risk of bias.”
Look at the evidence for yourself and decide if NICE were right to dismiss it all as they did. Look at the evidence for yourself and ask – can I (or my loved ones) really risk having low or insufficient vitamin D levels right now? Ask yourself – is there anything to lose by taking a vitamin D supplement for the foreseeable future and for my loved ones to do the same? (Ref 19). You may also like to ponder, as I found myself doing, why NICE would dismiss such a cheap, safe, and effective nutrient, which seems highly likely to help and does no harm.
Until the next time
All the best – Zoë
References
Ref 1: https://www.nice.org.uk/guidance/ng187/evidence/evidence-reviews-for-the-use-of-vitamin-d-supplementation-as-prevention-and-treatment-of-covid19-pdf-8957587789
Ref 2: https://www.zoeharcombe.com/2020/08/the-hierarchy-of-evidence/
Ref 3: Entrenas Castillo et al. Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study.; J Steroid Biochem Mol Biol. 2020.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7456194/
Ref 4: Annweiler et al. Vitamin D and survival in COVID-19 patients: A quasi-experimental study. 2020. The Journal of steroid biochemistry and molecular biology.
https://pubmed.ncbi.nlm.nih.gov/33065275/
Ref 5: Annweiler et al. Vitamin D Supplementation Associated to Better Survival in Hospitalized Frail Elderly COVID-19 Patients: The GERIA-COVID Quasi-Experimental Study. Nutrients. 2020.
https://pubmed.ncbi.nlm.nih.gov/33147894/
Ref 6: Hastie et al. Vitamin D concentrations and COVID-19 infection in UK Biobank. Diabetes & metabolic syndrome. 2020.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7204679/
Ref 7: Hernandez et al. Vitamin D Status in Hospitalized Patients With SARS-CoV-2 Infection. The Journal of Clinical Endocrinology & Metabolism. 2020.
https://academic.oup.com/jcem/advance-article/doi/10.1210/clinem/dgaa733/5934827
Ref 8: In COVID-19 patients, mean ± standard deviation 25OHD levels were 13.8 ± 7.2 ng/mL, compared with 20.9 ± 7.4 ng/mL in controls (P < .0001).
Ref 9: Karahan, S. and Katkat, F. Impact of Serum 25(OH) Vitamin D Level on Mortality in Patients with COVID-19 in Turkey. Journal of Nutrition, Health and Aging. 2020.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7533663/
Ref 10: The differences were quite striking 10.1 ± 6.2 vs. 26.3 ± 8.4 ng/mL, respectively, p<0.001.
Ref 11: Kaufman et al. SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels. PloS one. 2020.
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0239252
Ref 12: Macaya et al. Interaction between age and vitamin D deficiency in severe COVID-19 infection. Nutricion hospitalaria. 2020.
https://pubmed.ncbi.nlm.nih.gov/32960622/
Ref 13: Meltzer et al. Association of Vitamin D Status and Other Clinical Characteristics With COVID-19 Test Results. JAMA network open. 2020.
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2770157
Ref 14: Merzon et al. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study. The FEBS journal. 2020.
https://pubmed.ncbi.nlm.nih.gov/32700398/
Ref 15: Radujkovic et al. Vitamin D Deficiency and Outcome of COVID-19 Patients. Nutrients. 2020.
https://pubmed.ncbi.nlm.nih.gov/32927735/
Ref 16: Raisi-Estabragh et al. Greater risk of severe COVID-19 in Black, Asian and Minority Ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25(OH)-vitamin D status: study of 1326 cases from the UK Biobank. Journal of public health (Oxford, England). 2020.
https://academic.oup.com/jpubhealth/article/42/3/451/5859581
Ref 17: Ye et al. Does Serum Vitamin D Level Affect COVID-19 Infection and Its Severity? A Case-Control Study. Journal of the American College of Nutrition. 2020.
https://www.tandfonline.com/doi/full/10.1080/07315724.2020.1826005
Ref 18: https://www.zoeharcombe.com/2016/09/the-bradford-hill-criteria/
Ref 19: Eating a 200g tin of oily fish with the bones and skin will provide approximately 15mcg of vitamin D, which is a basic intake. Who consumes this daily? Sunbathing is a natural way to acquire vitamin D, but not possible for most people for many months of the year.
Continue reading...
Busting the cholesterol and saturated fat myths
This review article has been written because my peers and I believe that you have been completely misled and misinformed about the dangers of consuming saturated fat in the diet and the risks of developing heart disease.
It is by a combination of misinformation, poor scientific studies, corporate greed and deceptive marketing that has conspired to create one of the most damaging myths in medical history: that by consuming saturated fat in the diet and its effects on cholesterol you increase your risk of developing coronary heart disease (CHD). Sadly by following the mainstream advice for the last 30 years and eating a high carbohydrate low fat diet we now have an epidemic of obesity and type 2 diabetes in addition to high levels of heart disease.
As you will learn in this article, your total cholesterol levels are a poor predictor of heart disease; over 75% of patients admitted to hospital with a heart attack have perfectly normal total and LDL cholesterol levels and conversely at least 60 % of the people with high cholesterol numbers have perfectly healthy hearts (Malhotra 2017).
However around 66 % of patients admitted to hospital having a heart attack will have a condition known as “Metabolic Syndrome” – which is a cluster of CVD risk factors including elevated blood pressure, raised blood sugar, excess abdominal fat (enlarged waist girth), and low levels of HDL cholesterol and elevated Triglycerides (Malhotra 2017).
Since the 1980’s many of the ‘official’ dietary guidelines accepted and promoted by government and other health organisations warn us of the dangers of saturated fat “clogging up our arteries” – an analogy that has become ingrained in our subconscious, yet there is no convincing evidence that directly links dietary saturated with heart disease. We have been encouraged to remove fat from the diet and consume more carbohydrates despite the fact that there is plenty of evidence demonstrating an increased risk of heart disease from carbohydrate and sugar consumption resulting in hyperinsulinemia, insulin resistance, hypertension, weight gain, ‘pre’ & type 2 diabetes culminating in metabolic syndrome (Reaven et al, 2012).
Cholesterol has been wrongly demonised as a deadly substance that should be reduced by all means possible, conveniently enabling the pharmaceutical industry to make billions of pounds each year from ever increasing prescriptions of statins, despite their benefits being hugely over inflated through deceptive use of statistics and clever marketing. If the Pharmaceutical Industry succeeds in its mission, the majority of the population will be taking statins to prevent cardiovascular disease despite the fact that there isn’t any reliable, unbiased and non-industry funded research available to support such a plan. Sadly however modern western medicine has embraced a drug-based approach to combating all chronic disease prevention rather than encouraging patients to change their lifestyles such as adopting a High Fat Mediterranean diet and taking up regular exercise – both of which are far more powerful medicines in themselves without the unwanted side effects.
Why cholesterol is important:
- Cholesterol is one of the most vital molecules in the body; without it we would die
- Brain synapses – the vital connections between nerve cells in the brain are made almost entirely from
Cholesterol - Cholesterol forms an important constituent of all cell membranes
- Cholesterol is the basic raw material required to create Vitamin D. This highly important vitamin is not
only required to create healthy bones, protect against certain cancers, but has recently been identified as a having a protective effect on heart health – specifically coronary heart disease and heart failure. A recent study by Professor James Chong demonstrated that Vitamin D was able to reduce the amount of scar tissue (via its action on cardiac colony-forming unit fibroblasts) forming in the heart following a myocardial infarction (heart attack) and thus reducing the chances of impaired ‘pumping capacity’ as a result. Vitamin D deficiency is relatively common and under diagnosed especially during the winter months. - Sex hormones are created from Cholesterol such as Testosterone, Oestrogen and Progesterone
- Cholesterol is a key component of Bile which is released from the gall bladder to help with food digestion
At this point I think it’s important to point out that under normal circumstances LDL cholesterol – aka the “Bad Cholesterol” is not harmful until it becomes damaged through a process called oxidation which may result from toxins such as cigarette smoke, chronic stress or indeed when too much sugar is present in the bloodstream and creates damaged toxic molecules called advanced glycation end products (AGEs). Both of these processes contribute to chronic inflammation within the artery walls (endothelium) and ultimately coronary heart disease. Coronary heart disease is actually a chronic inflammatory disease that responds well to a high fat low carb Mediterranean diet.
The other important point to take note of is that a diet rich in sugar and refined carbohydrates will cause insulin resistance and will raise triglyceride levels – an important and independent risk factor for heart disease. So when you next have blood lipid profile test ask the doctor or nurse for a copy of your results. The two most important items you want to look at are your Triglycerides and HDL-c aka “Good” Cholesterol. According to leading preventative cardiologists your Triglyceride to HDL ratio is a much better predictor of heart attack risk than total cholesterol or LDL cholesterol. So your ideal would be fasting levels of HDL > 1.03 mmol/L for men and > 1.29 mmol/L for women and low levels of Triglycerides < 1.7 mmol/L both of which respond to dietary changes. Interestingly HDL-c levels increase rapidly when you add more healthy fats in the diet such as Extra Virgin Olive Oil and Virgin Coconut Oil – the latter being 90% saturated fat! Triglycerides can be lowered by both reducing refined carbohydrates and eating more Omega 3 Fatty Acids from oily fish (Malhotra 2017).
NB: Important Point on LDL Cholesterol
Conventional mainstream medical wisdom will tell you that eating a diet high in saturated fat will raise your LDL cholesterol (aka bad cholesterol) and increase your risk of developing coronary heart disease and Statins are prescribed primarily to lower your LDL cholesterol down to those ‘magic’ levels that NICE Guidance have set for us and the pharmaceutical industry strive to continuously lower. We all know this to be true right? – Well not exactly. You see when we first started hearing about the ‘evils’ of LDL – it was named “bad cholesterol” because doctors and researchers thought that is was the cholesterol that caused a build up of plaque in our arteries. However LDL itself isn’t actually cholesterol; it’s a ‘PARTICLE’ – The Low Density Lipoprotein (LDL) particle that is the ‘transport vehicle’ that contains the cholesterol and triglycerides within it and shuttles them around the bloodstream. So the concept of bad cholesterol is misleading as it’s actually the carrier particle (LDL) and the size of this particle that’s important – cholesterol itself appears to be an innocent bystander. To complicate matters – not all LDL particles are equally harmful or “atherogenic” which is a term used by doctors to describe something that drives the development of artery plaque or “atherosclerosis”. (Stick with me, we’re almost there on the technical stuff!) So basically some of our circulating LDL are large, buoyant particles (Type a) and some are small and dense (Type b)The small dense particles appear to be the atherogenic ones which we want to avoid. Because they are so small and dense they are able to penetrate the artery walls (endothelium) and begin the process of forming plaques. The large buoyant particles on the other hand appear to be harmless. So you may ask: Why am I telling you all of this? Ok, its important to understand because low fat carbohydrate rich diets not only lower HDL (good stuff) and raise triglycerides (bad stuff), they also create small dense LDL particles that are hazardous to our coronary arteries. All of these 3 factors increase our risk of heart disease.
NB: When however we eat a HIGH FAT LOW CARBOHYDRATE DIET the reverse is true: HDL increases, triglycerides decrease, and the circulating LDL becomes a large ‘fluffy’ harmless particle. Collectively these changes in response to diet decrease our risk of having a heart attack. To summarise: Consuming dietary saturated fat may raise cholesterol, but importantly it raises HDL cholesterol and the good part of LDL cholesterol (LDL- type A) far more than it raises the bad part of LDL cholesterol (LDL type B). There is no evidence that supports a direct relationship between saturated fat and heart disease (Sinatra 2017).
Also important to note that if you haven’t had a heart attack and don’t suffer from coronary heart disease taking a cholesterol lowering Statin drug will not prolong your life by a single day! FACT. However if you have suffered a heart attack taking a statin may benefit you whilst you remain high risk, and these benefits are most likely due to one its “pleiotropic effects” which are independent of cholesterol lowering. Statins do “other things” as cardiologists so eloquently say, although when you look at the absolute risk reductions over 5 years the benefits don’t look quite so impressive: 96% of patients saw no benefit at all, 1.2% of patients are prevented from death, 2.6% were helped by preventing another heart attack, and only 0.8% were prevented from having a stroke (NNT.com 2018). These figures are not what big pharma wants you to see, neither do they want you to know the potential side effects or harms caused: 2% of patients develop diabetes and 10% (reported) are harmed by muscle damage. Of course these common side effects are conveniently ‘swept under the carpet’.
So you may be wondering how and why have we been following this inaccurate nutritional advice for so long and where did this “fake news” come from in the first place?
Back in 1953 an American scientist named Ancel Keys published his now ‘infamous six countries study’ where he plotted on a graph the dietary fat intake of six countries against the numbers of deaths from heart disease. His graph showed a straight line relationship between higher fat intake and increased mortality (Figure 1).However, at the time of the study, there were data also available for another 16 countries. Keys chose to omit these 16 countries from his study because they did not fit his suggested linear relationship. Keys is responsible for the diet-heart hypothesis, which for many years has been the focus of heart attack prevention strategies around the world. It is important to note the word “hypothesis”. The fact is that these ideas have never actually been proven (only an association and not causality) and yet Keys’ research findings informed and were adopted by health organisations such as the American Heart Association (AHA), the British Heart Foundation (BHF) and government public health agencies in the UK despite the caveats of a British Doctor named John Yudkin who completely refuted Keys data. Yudkin’s much more comprehensive data showed that the single dietary factor that had the strongest association with coronary heart disease was indeed Sugar and not fat at all. Unfortunately Yudkin’s research was ridiculed at the time by the medical establishment (who had already made their minds up) and subsequently his ideas were ignored. Ironically his book “Pure White and Deadly – How Sugar is Killing us and what we can do about it” has recently been reprinted and become popular again today for good reason.
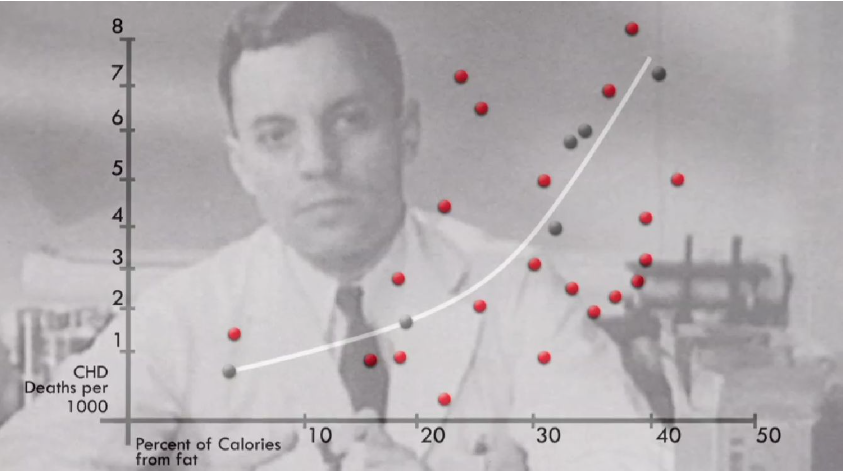
Figure 1. Graphic showing the six data points chosen by Keys in grey and the data Keys omitted as red points.
So let’s take a look at some of the recent evidence. The following passage has been taken from an editorial published in The British Journal of Sports Medicine (BJSM) last year (Aug 2017), and co- authored by Dr Aseem Malhotra – an outspoken Cardiologist, Anti – Sugar Campaigner and author of The Pioppi Diet who challenges conventional views on saturated fats and is a pioneer in the fight against sugar and its deleterious effects on health;
“Despite popular belief among doctors and the public, the conceptual model of dietary saturated fat clogging a pipe is just plain wrong.
A landmark systematic review and meta-analysis of observational studies showed no association between saturated fat consumption and ( 1) all-cause mortality, (2) coronary heart disease (CHD), (3) CHD mortality, (4) ischaemic stroke or ( 5) type 2 diabetes in healthy adults.(1) Similarly in the secondary prevention of CHD there is no benefit from reduced fat, including saturated fat, on myocardial infarction,
Cardiovascular or all-cause mortality. (2) I t is instructive to note that in an angiographic study of postmenopausal women with CHD, greater intake of saturated fat was associated with less progression of atherosclerosis whereas carbohydrate and polyunsaturated fat intake were associated with greater progression.( 3)
Shortly after this review findings were published from The PURE Study (6) which followed the dietary habits of 135,000 participants from 18 countries for 7 years and found that a high carbohydrate intake was associated with a higher risk of mortality (death), whereas total fat – including saturated fat were associated with lower risk of mortality. In addition all types of fat were not associated with cardiovascular disease, myocardial infarction (heart attack), or cardiovascular disease mortality. Stroke risk was inversely associated with saturated fat consumption – in other words eating saturated fat actually reduced risk of stroke. The paper concludes by saying “Global dietary guidelines should be reconsidered in light of these findings”.
In January this year (2018) David Chappell and I attended an Exercise Medicine Symposium in Cardiff – primarily as we wanted to hear the two keynote speakers – Dr Aseem Malhota and Professor Peter Brukner deliver their presentations on “You Can’t Outrun a Bad Diet” & “Why We Are Getting Fatter and Sicker”. Both experts explained how public health dietary messages have caused more harm than good and what we can do about it. More recently we both attended a conference in London for which the keynote speaker was Gary Taubes – an investigative journalist specializing in diet and nutrition and author of several books including “Why We Get Fat” and “The Case Against Sugar”. Gary’s history of the Diet-Heart Hypothesis left none of the audience (including many doctors) in any doubt that the dietary guidelines that are still current are based on fundamentally flawed research. He also presented the evidence for the benefits of switching to a High Fat Low Carb Diet.
Fortunately thanks to pioneering work of Dr Aseem Malhotra and many other supporting healthcare professionals – the tide is beginning to change. The Public Health Collaboration (PHC) is a charity that’s been set up by Samuel Feltham as an ‘antidote’ to Public Health England’s Eatwell Guide – that still promotes low fat foods and refined carbohydrates to the public. Overwhelming evidence has helped inform the creation of new healthy eating guidelines from the PHC Expert Panel and I am proud to have recently been appointed an ‘Ambassador for Brighton and Hove’ to help spread the word to the public, patients and healthcare professionals. These new healthy eating guidelines and weight loss advice handouts are now available from all Take Heart Classes as we want to give our members the best evidence based advice available so that they can achieve optimal health and fitness through our community cardiac rehab programmes in Sussex.
Meanwhile the government needs to accept responsibility that its recommendations for healthy eating and weight loss clearly haven’t worked. The UK has one of the highest prevalence of obesity in Europe at 25% and the number of people living with type 2 diabetes has more than doubled since 1996. Both cost the NHS £16 billion a year, and the UK economy at large £47 billion a year. These worrying statistics suggest that there is something wrong with the lifestyles of the UK population.
However, according to the latest National Diet and Nutrition Survey published in 2014 by PHE and the FSA adults in the UK have been generally following healthy eating guidelines. In fact on average adults in the UK have been eating 383 calories below the recommended daily amount as well as eating just below the recommended 35% for total fat consumption [7]. This paradox of the public following the “healthy eating” guidelines yet alarming health statistics showing otherwise brings into question the very guidelines that the UK population is being asked to follow. Many GP’s, nurses, pharmacists and sadly dieticians are still following these guidelines that frankly would be thrown out of court once the evidence had been heard against them.
The following Information is from thePublic Health Collaborations (PHC) Official Guidelines
Concern No 1: The Avoidance of Foods because of its Saturated Fat Content
The NHS Choices website recommends that people should “Go for lower-fat milk and dairy foods.”[15] This is based on the fact that full fat dairy foods contain higher amounts of saturated fat and under the Healthy dairy choices for adults section it says “A diet high in saturated fat can also lead to raised levels of cholesterol in the blood, and this can put you at increased risk of a heart attack or stroke.” The NHS Choices website also states under the Meat in your diet section that “Some meats are high in fat, especially saturated fat. Eating a lot of saturated fat can raise cholesterol levels in the blood, and having high cholesterol raises your risk of heart disease.” [16] Both recommendations were last updated in 2015 with review dates in 2017. However, well before then many analyses had been published finding that saturated fat is not an issue of concern. In March 2010 an analysis published in The American Journal of Clinical Nutrition by the Harvard School of Public Health followed 347,747 people over 5-23 years and concluded that ”Intake of saturated fat was not associated with an increased risk of coronary heart disease, stroke, or cardiovascular disease.” [ 17]
Following that in July 2012 a review published in the European Journal of Nutrition concluded that
“observational evidence does not support the hypothesis that dairy fat or high-fat dairy foods contribute to obesity or cardiometabolic risk, and suggests that high-fat dairy consumption within typical dietary patterns is inversely associated with obesity risk.”[18]
Finally, in March 2014 the University of Cambridge published an analysis in the Annals of Internal Medicine looking at a total of 643,226 people concluding that ”Current evidence does not clearly support cardiovascular guidelines that encourage high consumption of polyunsaturated fatty acids and low consumption of total saturated fats.” [19]
In fact a month after the advice from NHS Choices on meat was last reviewed in August 2015 an analysis of up to 339,090 people was published in the BMJ concluding that “Saturated fats are not associated with all-cause mortality, cardiovascular disease, coronary heart disease, ischemic stroke, or type 2 diabetes” [20]. Over a decade previously an analysis published in the BMJ by the Harvard School of Public Health in July 2003 followed 43,732 men over 14 years and concluded that “These findings do not support associations between intake of total fat, cholesterol, or specific types of fat and risk of stroke in men.” [21]
One of the most worrying aspects of the advice to lower fat consumption, and specifically saturated fat, was an analysis published in OpenHeart in February 2015 which looked at the evidence available in 1983 when the UK were first told to restrict fat concluded that “Dietary recommendations were introduced for 220 million US and 56 million UK citizens by 1983, in the absence of supporting evidence from randomised controlled trials.” [22]
In retrospect, there was never any strong evidence to recommend reducing total and saturated fat consumption and in the 30 years since the deteriorating health of the UK population suggests such advice may have been a dire mistake, however well intentioned. Quite possibly if the UK had been advised to go for foods in their natural form instead of unnaturally man-made low-fat foods for the past 30 years then there would not be such high rates of obesity, type 2 diabetes and cardiovascular disease, nor the associated social and financial costs they incur.
In light of this scientific evidence the Public Health Collaboration suggests that the UK stops recommending the avoidance of foods because of saturated fat content in order to focus on the consumption of food in its natural form, however much saturated fat it contains.
So if saturated fat isn’t bad for us but we know that sugar and refined carbs are – what should be eating? Enter the High FaMediterranean Diet…
The Lyon Heart study showed that adopting a Mediterranean diet in secondary prevention improved hard outcomes for both recurrent myocardial infarction (heart attack) and all-cause mortality (death) despite there being no significant difference in plasma low-density lipoprotein (LDL) cholesterol between the two groups. It is the alpha linoleic acid, polyphenols and omega-3 fatty acids present in nuts, extra virgin olive oil, vegetables and oily fish that rapidly attenuate inflammation and coronary thrombosis (blood clot in coronary artery)(6)
Here are the foods we advise cutting down on or eliminating from your diet (depending on disease status)
Bread, Potatoes, Pasta, Rice, Cereals (including granola and instant oats), crisps, biscuits and cakes, Fruit Juice, Soda’s, and high sugar content alcoholic drinks such as Beer although Red wine, Dry White Wine and spirits as they contain less sugar and can still be enjoyed in moderation. Beware of “FAKE FOODS” such as “low fat Foods” as they often contain added sugars – avoid them where possible – they are not healthy! Aim to eat Whole Unprocessed Foods.
Pioppi Diet Top Ten Foods (From The Pioppi Diet by Dr Aseem Malhotra)
- Extra Virgin Olive Oil (2-4 Tablespoons daily)
- Nuts (a handful daily ) Walnuts, hazelnuts, almonds
- Fibrous Vegetables including: Broccoli, Cauliflower, Courgettes, Aubergines, Onions, Sweet Potatoes
- Fruits including: tomatoes, avocados, apples, berries (blueberries, blackberries and raspberries)
- Herbs and Spices including: Garlic, Ginger, Turmeric, Basil and cinnamon.
- Fatty Fish for Omega 3’s including: Salmon, mackerel, sardines and anchovies
- Dark Chocolate ( 2 squares ) Preferably 85% cocoa solids
- Coconut (Cook freely with extra virgin coconut oil)
- Eggs (minimum of 10 each week)
- Full Fat and fermented dairy such as:(Greek FULL FAT Yogurt,Cheese and grass-fed butter)
R J Stantiford MSc., Dip H.ed, ACSM C-EP, BACPR cert
Continue reading...
Richard Stantiford co-founded The Lifestyle Physiologist in 2019 and works in Brighton and Hove and the surrounding areas.

Richard J Stantiford
Richard J Stantiford
MSc, Dip H.Ed, ACSM C-EP, BACPR, cert AAI
Richard is an Accredited Exercise Physiologist with 30 years’ experience in the health & fitness industry and is passionate about Lifestyle Medicine. He spent the first 10 years of his career working as a Personal Trainer in London’s most exclusive health clubs including “Champneys” of Piccadilly and coached a diverse range of clients including many celebrities. Whilst living in London he also completed 4 years training at the British School of Osteopathy where he learned an in-depth knowledge of anatomy, physiology and pathology, which included human cadaver dissection at Guys Medical School.
Richard is an appointed Public Health Collaboration (PHC) Ambassador for Brighton and Hove. The PHC are a Charity dedicated to informing and implementing healthier decisions for better public health. His role is to represent the PHC at a local level to nurture a network of people to help inform and implement healthier decisions (especially dietary advice) for where they live.
Richard is a Specialist Personal Trainer in Brighton and Hove. He provides Personal Training in Brighton to help clients lose weight and improve health outcomes offering both fitness classes and sessions in a training studio.
During his career Richard’s passion for knowledge in the field of Exercise Medicine has resulted in the acquisition of various Academic and Vocational Qualifications, which include:
Qualifications
- A Master’s (MSc.) Degree in Exercise and Behavioural Medicine (with distinction) from the University of West London
- National Diploma in Sport & Leisure Studies
- Higher Education Diploma in Osteopathy
- Certified Exercise Physiologist (C-EP) with the American College of Sports Medicine (ACSM C-EP) (Cert No: 513782)
- Accredited Phase IV Exercise Specialist with the British Association for Cardiac Prevention and Rehabilitation (BACPR)
- Accredited Pulmonary Rehab and Exercise Referral Specialist with the Wright Foundation.
- Accredited Rehab Trainer with Rehab Trainer (Australia)
- Certified Tai Chi and Qi Gong for Rehabilitation Instructor
- Immediate Life Support (ILS) trained (Resuscitation Council UK)
- Associate of the ARNI Institute for Stroke Rehabilitation (AAI)
- Diploma in LCHF Nutrition from The Noakes Foundation
Continuing Professional Development (CPD)
- BACPR – Physical Activity and Exercise in Heart Failure: Assessment, Prescription, and Delivery (2009)
- BACPR – Physical Activity and Exercise in the Management of Cardiovascular Disease Part II – Advanced Applications (2012)
- ACSM – Physical Activity Programming for Clients with Obesity (Feb 2017)
- ACSM – Polar Heart Rate Monitoring Assessment ( March 2017)
- BACPR – Assessing Functional Capacity: How to Administer and interpret Submaximal Tests in Clinical Populations (June 2017)
- Assessing Functional Capacity: How to administer and interpret Submaximal Tests in Clinical Populations (June 2017)
- ELITE HRV – Foundations of (HRV) Heart Rate Variability Course (November 2017)
- BACPR – Dietary Approach to Managing Cardiovascular Disease and Weight (November 2017)
- SCOPE – Specialist Certification of Obesity Professional Education (Core Learning Pathway) Part 1 (November 2017)
- Wales Exercise Medicine Symposium WEMS / BASEM (Jan 2018)
- Public Health Collaboration (PHC) Ambassador Training (February 2018)
- Balanced Approach – Tai Chi & QiGong CPD Update (November 2020)

Richard J Stantiford
Upon completion of his masters – Richard became an honouree lecturer at the University of West London teaching both undergraduate and graduate students Sport and Exercise Science.
For the last 15 years he has primarily focused on working with clients / patients who have underlying health problems, including cardiovascular, respiratory and metabolic conditions using a Lifestyle Medicine approach.
He currently divides his work between running a busy online (post Covid) cardiac rehab programme and working with private referred patients from Stroke Solutions in addition to helping complex obese patients on behalf of Sussex Medical Chambers. Richard has collaborated with some of the most influential medical experts in the UK including Consultant Cardiologist and best selling author Dr Aseem Malhotra, whom he refers patients that need specialist care.
Currently Richard is involved in a clinical research study at the Princess Royal Hospital working with acute stroke patients requiring upper limb physical therapy.
Richard provides services both online and in the community for cardiac rehabilitation, qi-gong and weight management.



